Collapsed Lung in Children: Care Instructions
Overview
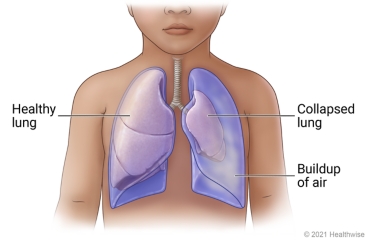
A collapsed lung (pneumothorax) is a buildup of air in the space between the lung and the chest wall. The pressure of the air against the lung makes the lung collapse. The lung cannot fully expand when your child inhales. This causes shortness of breath and chest pain.
A collapsed lung can be caused by an injury to the chest. But it may also occur suddenly because of a lung illness. A lung may collapse after lung surgery or another medical procedure. Sometimes it happens for no known reason.
Treatment can depend on the cause and severity of the collapsed lung. Treatment can also depend on whether the problem has returned. Your child may stay in the hospital for treatment. The lung may heal with rest, but the doctor will need to check your child. It can take several days for the lung to expand again. The doctor may have drained the excess air from your child's chest with a needle or tube. Surgery is sometimes done to keep the lung inflated.
The doctor will want to keep track of your child's progress. So your child will need a follow-up exam.
Your child may need further treatment if they are not getting better.
A collapsed lung may happen again. Watch for symptoms. If your child has shortness of breath or chest pain, get medical treatment right away.
Follow-up care is a key part of your child's treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse advice line (811 in most provinces and territories) if your child is having problems. It's also a good idea to know your child's test results and keep a list of the medicines your child takes.
How can you care for your child at home?
- Help your child get plenty of rest and sleep. Your child may feel weak and tired for a while, but your child's energy level will improve with time.
- Be safe with medicines. Read and follow all instructions on the label.
- If your child is not taking a prescription pain medicine, ask your doctor if your child can take an over-the-counter medicine.
- If the doctor gave your child a prescription medicine for pain, give it as prescribed.
- Store your child's prescription pain medicines where no one else can get to them. When you are done using them, dispose of them quickly and safely. Your local pharmacy or hospital may have a drop-off site.
- If the doctor prescribed antibiotics for your child, give them as directed. Do not stop using them just because your child feels better. Your child needs to take the full course of antibiotics.
- If your child has a bandage over the chest tube, or the place where the chest tube was inserted, keep it clean and dry. Follow your doctor's instructions on bandage care.
- If your child goes home with a tube in place, follow the doctor's directions. Do not adjust the tube in any way. This could break the seal or cause other problems. Keep the tube dry.
- Do not let your child exercise until your doctor says it's okay.
- Do not let your child fly in an airplane or scuba dive until your doctor tells you it is okay.
- Keep your child away from smoke. Do not smoke or let anyone else smoke around your child or in your house.
When should you call for help?
Call 911 anytime you think your child may need emergency care. For example, call if:
- Your child has severe trouble breathing.
- Your child has severe chest pain.
- Your child passes out (loses consciousness).
Call your doctor or nurse advice line now or seek immediate medical care if:
- Your child has new or worse trouble breathing.
- Your child has new or worse pain.
- Your child coughs up blood.
- Your child's chest tube comes out or is bent or blocked.
- Your child is bleeding through the bandage where the tube was put in.
- Your child has symptoms of infection where the tube was put in, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Watch closely for changes in your child's health, and be sure to contact your doctor or nurse advice line if:
- The skin around the place where the chest tube was put in is red or irritated.
- Your child does not get better as expected.
Where can you learn more?
Go to https://www.healthwise.net/patientEd
Enter N773 in the search box to learn more about "Collapsed Lung in Children: Care Instructions".
Current as of: July 31, 2024
