Anemia: Care Instructions
Overview
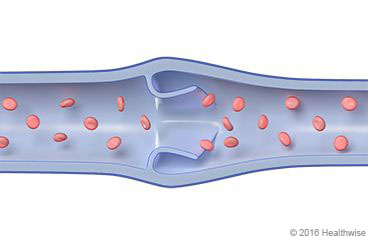
Anemia is a low level of red blood cells, which carry oxygen throughout your body. Many things can cause anemia. Lack of iron is one of the most common causes. Your body needs iron to make hemoglobin. This is a substance in red blood cells that carries oxygen from the lungs to your body's cells. Without enough iron, the body produces fewer and smaller red blood cells. As a result, your body's cells do not get enough oxygen, and you feel tired and weak. And you may have trouble concentrating.
Bleeding is the most common cause of a lack of iron. You may have heavy menstrual bleeding or bleeding caused by conditions such as ulcers or cancer. Regular use of aspirin or other anti-inflammatory medicines (such as ibuprofen) also can cause bleeding in some people. A lack of iron in your diet also can cause anemia, especially at times when the body needs more iron. This includes during pregnancy, infancy, and the teen years.
Your doctor may have prescribed iron pills. It may take several months of treatment for your iron levels to return to normal. Your doctor also may suggest that you eat foods that are rich in iron, such as meat and beans.
There are many other causes of anemia. It is not always due to a lack of iron. Finding the specific cause of your anemia will help your doctor find the right treatment for you.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse advice line (811 in most provinces and territories) if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
- Take your medicines exactly as prescribed. Call your doctor or nurse advice line if you think you are having a problem with your medicine.
- If your doctor recommends iron pills, take them as directed:
- Try to take the pills on an empty stomach about 1 hour before or 2 hours after meals. But you may need to take iron with food to avoid an upset stomach.
- Do not take antacids or drink milk or caffeine drinks (such as coffee, tea, or cola) at the same time or within 2 hours of the time that you take your iron. They can make it hard for your body to absorb the iron.
- Vitamin C (from food or supplements) may help your body absorb iron. Some people take iron pills with a glass of orange juice or some other food that is high in vitamin C, such as citrus fruits.
- Iron pills may cause stomach problems, such as heartburn, nausea, diarrhea, constipation, and cramps. Be sure to drink plenty of fluids, and include fruits, vegetables, and fibre in your diet each day. Iron pills often make your bowel movements dark or green.
- If you forget to take an iron pill, do not take a double dose of iron the next time you take a pill.
- Keep iron pills out of the reach of small children. An overdose of iron can be very dangerous.
- Your doctor may recommend eating more iron-rich foods. These include red meat, poultry, eggs, beans, raisins, whole grain bread, and leafy green vegetables. Some fortified cereals and grains are high in iron.
When should you call for help?

Call 911 anytime you think you may need emergency care. For example, call if:
- You have symptoms of a heart attack. These may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Light-headedness or sudden weakness.
- A fast or irregular heartbeat.
After you call 911, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself. - You passed out (lost consciousness).
- You have severe shortness of breath.
Call your doctor or nurse advice line now or seek immediate medical care if:
- You have new or increased shortness of breath.
- You are dizzy or light-headed, or you feel like you may faint.
- You have new or worse nausea and vomiting.
- Your fatigue and weakness continue or get worse.
- You have any abnormal bleeding, such as:
- Nosebleeds.
- Vaginal bleeding that is different (heavier, more frequent, at a different time of the month) than what you are used to.
- Bloody or black stools, or rectal bleeding.
- Bloody or pink urine.
Watch closely for changes in your health, and be sure to contact your doctor or nurse advice line if:
- You do not get better as expected.
Where can you learn more?
Go to https://www.healthwise.net/patientEd
Enter R301 in the search box to learn more about "Anemia: Care Instructions".
Current as of: October 7, 2024
