Condition Basics
What is sickle cell disease?
Sickle cell disease is a genetic red blood cell disorder. It changes normal, round red blood cells into cells shaped like crescent moons. Sickled cells can get stuck in blood vessels and block them, which stops oxygen from getting through. That can cause a lot of pain and can harm organs, muscles, and bones.
How does it affect your body?
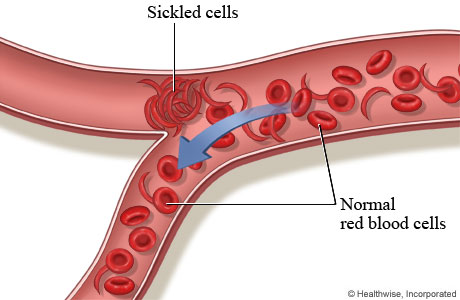
Normal red blood cells move easily through blood vessels, taking oxygen to every part of your body.
People who have sickle cell disease have mostly sickled red blood cells. These cells can get stuck and block blood flow through a blood vessel. That means red blood cells and oxygen can't flow to some parts of the body.
What causes sickle cell disease?
Sickle cell disease is inherited, which means it is passed from parent to child. To get sickle cell disease, a child has to inherit two sickle cell genes—one from each parent. These sickle cell genes are defective hemoglobin S genes.
What are the symptoms?
Painful events (sickle cell crises) in the hands or feet, belly, back, or chest are the most common symptom of sickle cell disease. This pain may last from hours to days. Most people with sickle cell disease are anemic, which can make them feel weak and tired.
How is it diagnosed?
Sickle cell disease is diagnosed when a blood test shows abnormal hemoglobin. Your doctor might order more tests.
Infants may be screened for the disease before they go home from the hospital. This sickle cell test looks for sickle cell trait and an increased risk of sickle cell disease.
How is sickle cell disease treated?
Treatment involves getting routine tests to monitor health, managing pain events (sickle cell crises) with medicine, and treating related health problems as they arise. Some people need regular blood transfusions to lower the risk of stroke and to treat anemia and other problems.
Cause
Sickle cell disorders are inherited. That means they are passed from parent to child. Children with sickle cell disease have two defective hemoglobin S genes, one from each parent. Various forms of sickle cell disorders occur when a person inherits one hemoglobin S gene (sickle cell gene) from one parent and one other type of defective hemoglobin gene from the other parent.
Normally, a person inherits two genes that tell the body to produce normal hemoglobin A. One gene comes from each parent. People who inherit one defective hemoglobin S gene and one normal hemoglobin A gene have sickle cell trait. These people rarely have symptoms of sickle cell disease. Their bodies don't make sickled blood cells. But, as carriers, they can pass the defective hemoglobin S gene to their children.
Symptoms
When a child is born with sickle cell disease, no one can predict which symptoms will appear, when they will start, or how bad they will be.
Painful events (sickle cell crises) in the hands or feet, belly, back, or chest are the most common symptom of sickle cell disease. They are periods of pain that happen when sickled cells get stuck in blood vessels and block the blood flow. This pain may last from hours to days.
Most people with sickle cell disease are anemic. Anemia can make you feel weak and tired. People with sickle cell anemia may look pale or washed out. They may be short of breath. Their skin and the whites of their eyes may have a yellowish look (jaundice).
What Happens
When a child is born with sickle cell disease, it's impossible to predict which problems will develop, when they will start, or how bad they will be. During the first 6 months of life, infants have a high level of fetal hemoglobin (HbF) in their blood, which protects them from red blood cell sickling. But dangerous complications of sickle cell disease may quickly develop between ages 6 months and 5 years, after levels of fetal hemoglobin decrease.
Older children and adults with sickle cell disease may have few problems. Or they may have a pattern of ongoing complications that shortens their lives. The most common and serious problems caused by sickle cell disease are anemia, pain, and organ failure.
Complications
Sickle cell disease may cause problems such as:
- Anemia, pain, and organ failure. These are the most common and serious problems.
- Sickle cell crisis. This is a common and painful problem that happens when blood vessels are blocked.
- Splenic sequestration. Large, sickled blood cells get trapped in the spleen. It can cause sudden and life-threatening anemia.
- Acute chest syndrome. Symptoms include coughing and chest pain.
- Severe infections.
- Aplastic crisis. The bone marrow stops producing red blood cells. This causes sudden, severe anemia.
- Stroke.
Other problems include:
- Growth slowdown. Children who have sickle cell disease often grow more slowly than normal and go through puberty later.
- Open sores on the legs and feet. These sores can be very painful and heal slowly.
- Eye damage. Long-term vision problems, including blindness, may result from blocked blood flow in the inner lining of eye.
- Pulmonary hypertension. This means blood pressure is very high in the lungs.
Learn more
When to Call a Doctor
Call 911 or other emergency services immediately if you have sickle cell disease and have:
- Trouble breathing or shortness of breath.
- Chest pain.
- Severe belly pain.
- Sudden weakness.
- Sudden numbness or tingling in the hands, feet, fingers, or toes (even if it goes away on its own).
- Sudden poor balance and poor coordination when walking (even if it goes away on its own).
- Confusion (even if it goes away on its own).
- Garbled speech or an inability to speak (even if it goes away on its own).
- Sudden change in vision.
- Severe headache.
- Loss of consciousness.
- Fever.
- Severe cough.
- Repeated vomiting or persistent diarrhea.
- A sudden increase in the size of your or your child's spleen. (Learn from your doctor how to feel your child's spleen to check its size.)
- Increased paleness.
- Light-headedness.
- Persistent erection of the penis (priapism) that lasts more than 2 to 3 hours or is extremely painful.
- Severe pain that can't be relieved with your usual prescription pain medicines or other pain-relief methods.
Call your doctor if you or your child has:
- A painful event (sickle cell crisis).
- An open sore (ulcer) on the leg.
- More frequent urination than usual.
Make a pain management plan with your doctor that includes where and when to get treatment in case of a sickle cell emergency.
Learn more
Exams and Tests
Sickle cell disease is diagnosed when initial blood tests show abnormal hemoglobin. More tests might be needed depending on the results.
As part of Alberta's newborn screening, the disease can be screened for as early as 24 hours after birth. A sickle cell screen looks for sickle cell trait and an increased risk of sickle cell disease. A sample of blood is taken from the infant's heel. It's sent to a lab. There it is screened for the presence of sickle cell hemoglobin (hemoglobin S). If an infant is at increased risk for sickle cell disease, more diagnostic tests might be arranged.
Testing people who are planning to become pregnant for sickle cell disease (parental sickle cell disease tests) can help identify if a couple is at risk of having a baby with sickle cell disease. Both partners should talk to their doctor about their family history of sickle cell disease or sickle cell trait. Couples who are at risk for passing on this disease to their children may want to talk with a genetic counsellor about prenatal testing before getting pregnant.
Doctors can also diagnose sickle cell disease before a child is born (prenatally). Prenatal tests include amniocentesis and chorionic villus sampling (CVS). Your doctor will likely order parental sickle cell disease tests first, before prenatal testing.
Learn more
Treatment Overview
Medical treatment can help you manage pain and avoid other health problems from sickle cell disease.
Early treatment includes daily antibiotics from 2 months to 5 years of age to help prevent infections. Routine childhood and adult immunizations are also important. Your doctor may also suggest you take folic acid supplements.
Medicines that treat sickle cell disease include hydroxyurea and pain medicines. You may need a prescription for some of the medicines. Others you can buy over-the-counter. Pain medicine may work best when you also do other things to manage pain. You can prepare for painful events ahead of time by creating a pain management plan with your doctor.
Some people need regular blood transfusions to lower the risk of stroke and to treat anemia and other problems. Some people take prescription medicine, such as L-glutamine (Endari), to prevent problems. In rare cases, a stem cell transplant might be an option.
Treating pain
In many cases, you can treat mild to severe sickle cell pain at home. You can use a combination of pain medicines, plenty of fluids, and comfort measures such as heating pads or hot water bottles. Do not use heating pads with children.
A painful event (crisis) can become severe and may last for days to weeks. If home treatment doesn't help enough, you'll need strong pain medicine that must be monitored in a hospital or treatment centre.
Learn more
Watch
Self-Care
Here are some things you can do to help prevent problems when you or your child has sickle cell disease.
- Make and follow a plan for how to treat pain.
Work with your doctor to make a plan that includes instructions on how to treat pain at home. Your plan should also tell you when you need to go to the hospital if your pain gets worse.
- Avoid infections.
Make sure that you and your child get all the recommended vaccines on schedule.
To help your child with sickle cell disease, make sure that your child takes antibiotics until age 5. And help your child avoid contact with anyone who might have fifth disease. A virus that causes fifth disease can suddenly stop the body from producing red blood cells. This is called an aplastic crisis.
- Get routine eye exams.
Eye exams can find problems early.
- Drink water and other fluids to prevent dehydration.
- Drink extra fluids before, during, and after exertion and when you're in the heat.
- Drink plenty of fluid if you have a fever or infection.
- Limit alcohol.
- Children should keep a water bottle with them during school, play, and outings.
- Eat healthy foods.
Healthy eating helps keep your body's immune system strong. Talk to your doctor about what foods can help you stay healthy and any dietary supplements you may need. These are often a necessary part of the diet for people with sickle cell disease. They're even more important if you aren't eating enough folate-rich leafy vegetables (such as spinach).
- Don't smoke.
Smoking and second-hand smoke reduce the amount of oxygen in your bloodstream.
- Exercise safely.
- Rest when you feel tired.
- Drink plenty of fluids when you exercise. Strenuous exercise can cause dehydration and reduced oxygen levels in your blood. This may cause red blood cells to sickle.
- Children can exercise and play normally if they:
- Stay hydrated.
- Take rest breaks.
- Stay warm. Being exposed to cold air, wind, and water can trigger a sickle cell crisis. Dress children in warm layers of clothing for cold-weather activities. Avoid swimming and playing in cold water.
- Stay safe at high altitudes and during air travel.
Low oxygen levels caused by high altitudes and plane flights can cause problems. To avoid problems, drink plenty of water and fluids during air travel or when you're at altitudes higher than 1500 m (5000 ft), such as in the mountains.
- Recognize serious symptoms.
Talk to your doctor about what symptoms to watch for. And know when to call your doctor and when you need emergency help.
Treating pain
If you have sickle cell disease, you can take steps to treat pain at home.
- Use a hot water bottle or a heating pad set on low.
Do not use a heating pad when you are in bed. You may fall asleep and burn yourself.
- Learn pain-management skills.
These can help take the focus off of the pain, or they can help the pain medicine work better. You can work with a pain specialist to learn about different techniques, such as:
- Guided imagery. This process uses your senses to guide your imagination into a more relaxed state.
- Progressive muscle relaxation. This process helps you relax your muscles, which can help lower tension and anxiety.
- Distraction.
- Deep breathing.
- Positive, encouraging self-talk.
- Use pain medicines.
You and your doctor can make a pain management plan. You're probably the best judge of when you need to use a stronger medicine.
- For mild pain, use over-the-counter ibuprofen (such as Advil), acetaminophen (such as Tylenol), or both.
- For moderate or severe pain, you might take pain medicine prescribed by your doctor. Prescription pain medicine includes oral medicines such as codeine and ibuprofen, or codeine and acetaminophen. Some people might take oral controlled-release morphine at home.
Managing your child's at-school needs
You can take steps to help your child cope at school with the special needs of having sickle cell disease.
- Help your child keep up in school.
Make arrangements with teachers or a tutor to help your child keep pace with classmates when illness causes absences from school.
- Talk with your child's teachers about washroom breaks.
Explain that children with sickle cell disease may need to use the washroom more often than other kids. They also need more water than the other students. Not drinking enough water can raise the chance of a sickle cell crisis.
- Give school staff members instructions about what to do in an emergency.
Educate teachers and other school employees about the signs and symptoms of sickle cell disease that need urgent medical care. Write down the instructions and list who to call in an emergency.
- Take steps to help your child safely exercise and play at school.
- Have your child drink plenty of fluids before, during, and after exercise. Lack of fluids (dehydration) can cause cells to sickle.
- Encourage your child to get regular rest breaks during vigorous exercise.
- Remind your child to stay warm. Exposure to cold air, wind, and water can trigger a sickle cell crisis. Dress your child in warm layers of clothing for cold-weather activities. Your child should avoid swimming and playing in cold water.
Learn more
Watch
Credits
Adaptation Date: 02/24/2022
Adapted By: Alberta Health Services
Adaptation Reviewed By: Alberta Health Services
