Overview
Breastfeeding is feeding a baby milk from your breasts. You can also pump your breasts and put the milk in a bottle to feed your baby. Breast milk is the only food that babies need for the first 6 months of life. At around 6 months of age, you can start slowly adding other foods, such as iron-fortified infant cereal, while your baby continues to breastfeed.
Experts such as the Canadian Paediatric Society, Health Canada, and the American Academy of Pediatrics (AAP) recommend feeding your baby only breast milk for about 6 months. They also support breastfeeding for 2 years or longer.footnote 1, footnote 2 But your baby benefits from any amount of time that you breastfeed. Try to breastfeed for as long as it works for you and your baby.
Breastfeeding has many benefits. It may lower your baby's chances of getting an infection. It also may make it less likely that your baby will have problems such as diabetes and obesity later in life. Breastfeeding also helps you bond with your baby.
In the first days after birth, your breasts make a thick, yellow liquid called colostrum. This liquid gives your baby nutrients and antibodies against infection. It's all that babies need in the first days after birth. Your breasts will fill with milk a few days after the birth.
Breastfeeding is a skill that gets better with practice. Be patient with yourself and your baby. If you have trouble, you can get help and keep breastfeeding.
How can you prepare for breastfeeding?
The more you prepare and learn about breastfeeding now, the more likely it will go well. So talk to your doctor or midwife, and ask questions now. Take a class to learn about breastfeeding and how it's done best. And ask about lactation consultants at your hospital or birthing centre.
How often should you breastfeed?
Plan to breastfeed your baby on demand rather than setting a strict schedule. For the first 2 weeks, be prepared to breastfeed at least 8 times in a 24-hour period. In the first few days, you may need to wake a sleeping baby to feed. If you breastfeed more often, it will help your breasts produce more milk.
By 2 months, most babies have a set feeding routine. But your baby's routine may change at times, such as during growth spurts when your baby may be hungry more often.
At around 3 months of age, your baby may breastfeed less often. That's because your baby is able to drink more milk at one time. Your milk supply will naturally increase as your baby needs more milk.
What should you know about your first feeding?
It's best to start breastfeeding within 1 hour of birth. For each feeding, you go through these basic steps:
- Get ready for the feeding. Be calm and relaxed, and try not to be distracted. Get some water or juice for yourself. Use two or three pillows to help support your baby while nursing.
- Find a breastfeeding position that is comfortable for you and your baby. Examples are the cradle and the football positions. Make sure the baby's head and chest are lined up straight and facing your breast. It's best to switch which breast you start with each time.
- Get the baby latched on well. Your baby's mouth needs to be wide open, like a yawn. So you may need to gently touch the middle of your baby's lower lip. When your baby's mouth is open wide, quickly bring the baby onto your nipple and areola. The areola is the dark circle around your nipple.
- Provide a complete feeding. Let your baby decide how long to nurse. Be sure to burp your baby after each breast.
In the first days after birth, your breasts make a thick, yellow liquid called colostrum. This liquid gives your baby nutrients and antibodies against infection. It is all that babies need at first. Your breasts will fill with milk a few days after the birth.
Talk to your doctor, midwife, public health nurse, or lactation consultant right away if you are having problems and aren't sure what to do.
Does your baby need extra vitamins or minerals?
Doctors sometimes prescribe vitamin or iron drops for newborns. These drops help babies get the nutrition they need.
A baby may need:
- Vitamin D. Breast milk does not have a lot of vitamin D. Breastfed babies need 400 IU of vitamin D each day from vitamin D drops. And formula-fed babies may also need vitamin D drops, depending on how much formula they drink.
- Iron. Babies born early haven't had enough time to build up an iron supply before birth. So they usually get iron drops for the first year after birth.
- Vitamin K. All newborns should receive vitamin K in the first 6 hours after birth to lower the risk of severe bleeding. Learn more about vitamin K for newborns.
If you have questions, talk with your doctor about what is right for your baby.
Benefits of Breastfeeding
Breast milk may help protect your child from some health problems.
- Breastfed babies are less likely than formula-fed babies to:
- Get ear infections, colds, diarrhea, and pneumonia.
- Be obese or get diabetes later in life.
- Breastfeeding your child may also help prevent sudden infant death syndrome (SIDS).
Breastfeeding has benefits for you too. It causes the release of a hormone called oxytocin. This hormone may help your uterus shrink back faster. And breastfeeding can lower your risk of breast cancer, ovarian cancer, and osteoporosis.
Planning
Before your baby is born, plan ahead. Learn all you can about breastfeeding. This helps make breastfeeding easier.
- Early in your pregnancy, talk to your doctor, midwife, or public health nurse about breastfeeding.
- Learn the basics before your baby is born. The staff at hospitals and birthing centres can help you find a lactation consultant. This person is often a nurse who has been trained to teach and advise about breastfeeding. Or you can take a breastfeeding class.
- Plan ahead for times when you will need help after your baby is born. You may want to get help from friends and family. You can also join a support group to talk to others who breastfeed.
- Buy the equipment you'll need. Examples are breast pads, nipple cream, extra pillows, and nursing bras. Find out about breast pumps too.
Learn more
Watch
How to Breastfeed
Here is a step-by-step guide on how to breastfeed. It shows one position that you can use for breastfeeding. There are other positions you can try. Talk to your doctor, midwife, or lactation consultant if you have trouble getting your baby to latch on.
How do you breastfeed?
- Get ready.

Find a place to sit where you feel relaxed and comfortable. Make sure your back is supported. Try using a pillow on your lap to support your baby.
- Try supporting your breast with one hand.
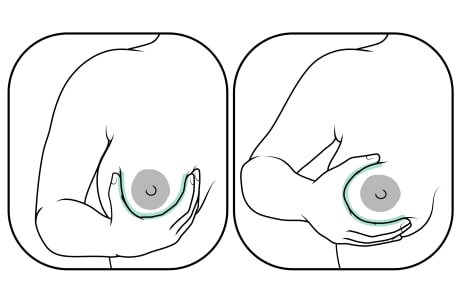
- U hold: Your thumb is on the outer side of your breast. Your fingers are on the inner side.
- C hold: Your thumb is above the darker area around the nipple (areola). Your fingers are below.
- Use your other hand and arm to hold your baby.

Support the base of their head.
- Try different positions if you need to.

Find what works for you and your baby. Different holds include cradle, cross-cradle, football, Australian, laid back, and side-lying.
- Help your baby latch.
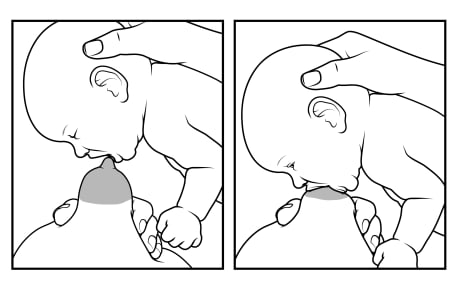
Touch your baby's lower lip with your nipple. Wait until your baby's mouth opens wide. Bring your baby quickly to your breast, and guide your breast into their mouth.
- Look for a good latch.
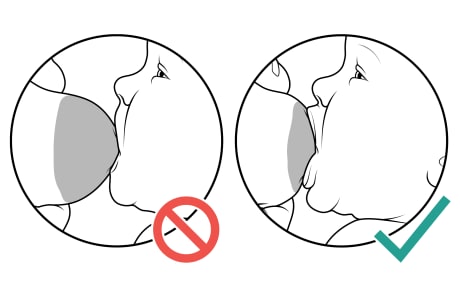
Make sure that your nipple and much of your areola are in your baby's mouth. Your baby's lips are flared out, not folded in.
- Listen for regular sucking and swallowing sounds.
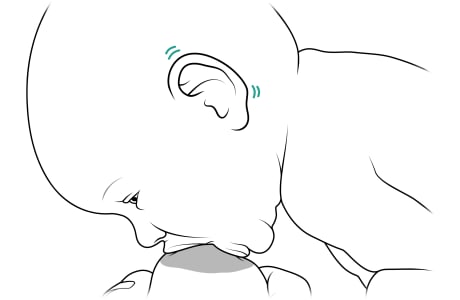
If you can't see or hear swallowing, watch your baby's ears. They'll wiggle slightly when your baby swallows.
- Break the latch if you need to.

Put one finger in the corner of your baby's mouth between your breast and your baby's gums. This helps prevent cracking and painful nipples.
What are some tips for breastfeeding?
These tips can help you succeed as you get used to breastfeeding your newborn.
- Breastfeed your baby whenever your baby is hungry. In the first 2 weeks, your baby will breastfeed at least 8 times in a 24-hour period.
- Hold your baby in a comfortable position. Try different positions, such as the cradle hold and football hold.
- Help your baby to latch on properly.
- Touch your baby's lower lip with your nipple until your baby's mouth opens wide.
- Make sure that your baby's mouth covers a lot of the areola and that the lips are flared out.
- Listen for deep, rhythmic sucking sounds.
- Each time you breastfeed, switch which breast you start with.
- Break the baby's latch on your breast before moving your baby. Push your finger between your baby's gums to gently break the seal.
- Burp your baby after each breast. Gently pat your baby's back to let out any swallowed air.
Learn more
Watch
Your Health and Nutrition
After the birth, it'll be important to take good care of yourself—by resting when you can, having good support, and staying healthy. Consider asking someone to stay with you to help for a few days. At first, plan to limit your guests and how long they stay, so you can rest.
Eating well during breastfeeding will help you stay healthy. A healthy diet includes eating a variety of vegetables and fruits, whole grain foods, and protein foods.
Learn what to avoid, such as fish that are high in mercury. These include shark and some types of tuna. And limit alcohol and caffeine. They can pass to your baby through breast milk.
If you are breastfeeding, your doctor or midwife may suggest eating more calories each day than otherwise recommended for a person of your height and weight.
Learn more
Your nutrition
Your health
Pumping and Storing
Pumping and storing your milk allows your baby to get breast milk from a bottle. It's a good idea to have a plan for when you'll need to pump, select the right breast pump for you, and know how to store milk safely. This will help set up you and your baby for long-term success.
- Chose a breast pump. There are many types of pumps that you can get. You'll want to think about which kind is most practical for how often you'll need to use it.
- Plan ahead to pump at work. Think about where you can pump and how often you'll need to pump. Regular pumping will help ensure that your breasts produce enough milk. It will also keep your breasts from becoming uncomfortable and engorged.
- Learn how to store breast milk properly. Stored breast milk is the next best thing to fresh breast milk. There are steps you can take to safely prepare breast milk for storage and guidelines for how long you can keep it.
What if you have problems or concerns?
If you have problems using a breast pump or have concerns about your milk supply, talk to a lactation consultant.
Learn more
Watch
Common Problems
It's common to have struggles sometimes when you're breastfeeding. Most breastfeeding issues can be solved when you know what to expect and have support from others, including your doctor, midwife, or lactation consultant.
Here are some common problems and some tips for working through them.
- Sore or cracked nipples. Although sore or tender nipples are common during the first few days of breastfeeding, this should improve. Allow some breast milk to dry on your nipples. Breast milk contains natural skin softeners and antibodies to fight infection. This can help heal nipples and keep them healthy. To help prevent problems, make sure your baby is latching on correctly. Change your baby's position with each feeding. And be sure to break the latch before removing your baby from your breast.
- Engorged breasts. Breasts that are overfull of milk (engorged) can be painful and can make it hard for your baby to breastfeed. If engorgement becomes severe, it can lead to a breast infection. Soften your breasts before feedings by using a warm compress for a few minutes. Or use your hands or a pump to let out (express) a small amount of milk from both breasts. Your doctor may suggest taking ibuprofen (such as Advil or Motrin). You can also try cool compresses to reduce swelling.
- Blocked milk ducts. Blocked milk ducts cause a lump that is sometimes tender and can become infected (mastitis). Milk ducts in the breast may become blocked when the breasts are full and not emptied regularly or completely. Breastfeed more often and in different positions to help drain milk from all parts of the breast. Breastfeed from the affected breast first, to move milk through the breast faster. You can also apply moist heat to the area just before breastfeeding, and hand-express or pump a small amount of milk.
- Mastitis. Mastitis is a painful inflammation of the breast. The area may be red or warm to the touch. And you may have a fever and chills, aches, and flu-like symptoms. Treatment includes taking antibiotics and regularly emptying your breast by breastfeeding or pumping your breast milk. (When you have mastitis, your milk is still safe for your baby to drink.) Self-care includes taking acetaminophen (such as Tylenol) and using hot or cold compresses to ease your discomfort. Treating mastitis right away helps keep the infection from getting worse and usually eases symptoms.
- Fungal infection (thrush). A thrush infection in your baby can cause white patches in the baby's mouth, a sore mouth, and a diaper rash. If your nipples become red and sore, or if you have breast pain during or after breastfeeding, it may be a sign that a thrush infection in your baby has spread to your nipples. Thrush is treated with a prescription antifungal medicine such as nystatin. It can be given as a liquid that's put on the white patches in the mouth and on your nipples or as a cream or ointment for the diaper area.
- Low milk supply. It's common to worry about not making enough milk. But low milk supply is rare. It may take time for your milk supply to get going. Breastfeeding stimulates your body to make milk. So the more often you feed your baby and empty your breasts, the more milk your body makes. If you don't think your baby is getting enough milk, try breastfeeding more often. If this doesn't help, talk to your doctor, midwife, or lactation consultant.
- Problems with let-down: When your breasts are stimulated by breastfeeding or pumping, this causes milk to move from the milk ducts and out through the tiny holes in the nipple. This is called the let-down reflex. If your let-down reflex is strong, milk may flow too quickly and your baby may have trouble swallowing it. Try leaning back and nursing "uphill" so that your baby is above the nipple. If your let-down is weak, your nipples may get sore if your baby sucks more strongly to try to get milk. Express a little milk from your breasts right before a feeding. This can help with the let-down reflex. And focus on being comfortable and relaxed at each feeding.
Learn more
Watch
When to Call a Doctor
Call your doctor now if you have:
- Increasing pain in one area of the breast.
- Increasing redness in one area of the breast or red streaks extending away from an area of the breast.
- Drainage of pus from the nipple or another area of the breast.
- A fever of 38.3°C (101°F) or higher.
Call your doctor today if you have:
- Breast problems, such as cracked and bleeding nipples or blisters on your nipples, that are not relieved by home treatment.
- A fever less than 38.3°C (101°F).
- Symptoms of postpartum depression, such as often feeling sad, tearful, anxious, hopeless, or irritable. Postpartum depression can make breastfeeding problems seem even worse.
- Swollen glands (lymph nodes) in your neck or armpit.
Call your doctor today if your baby:
- Is not eating well for any reason or has:
- A rectal temperature of 38°C (100.4°F) or higher.
- Fussiness or sleepiness that interferes with breastfeeding.
- Weakness, listlessness, or lack of interest in feeding.
- Thick, white patches in the mouth and cheeks. These are signs of a yeast infection (thrush), or signs of a diaper rash.
- Shows signs of poor eating, such as:
- Not reaching their birth weight by 2 weeks of age or gaining weight too slowly after 2 weeks of age.
- Having no wet diapers for 6 hours.
- Passing little or no stool over a 24-hour period in the first 4 weeks, or passing stools that are dark green and contain mucus after the first few days. But it's normal for your baby to have fewer stools starting around 4 to 8 weeks of age. As long as stools stay soft and your baby is feeding well, it should not be a concern.
- Having problems latching on to the breast.
References
Citations
- Health Canada, et al. (2012). Nutrition for healthy term infants: Recommendations from birth to six months. A joint statement of Health Canada, Canadian Paediatric Society, Dietitians of Canada, and Breastfeeding Committee for Canada. Available online: http://www.hc-sc.gc.ca/fn-an/nutrition/infant-nourisson/recom/index-eng.php.
- American Academy of Pediatrics (2022). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 125(1): 1–15. DOI: 10.1542/peds.2022-057988. Accessed July 18, 2022.
Credits
Adaptation Date: 09/19/2025
Adapted By: Alberta Health Services
Adaptation Reviewed By: Alberta Health Services
