Condition Basics
What are functional ovarian cysts?
A functional ovarian cyst is a fluid-filled sac that forms on an ovary. A sac normally forms during ovulation to hold a maturing egg. Usually the sac goes away after the egg is released. But if an egg isn't released, or if the sac closes up after the egg is released, the sac can swell up with fluid.
During the normal monthly menstrual cycle, one of two types of functional cysts may form.
- A follicular cyst. This type occurs when a sac on the ovary doesn't release an egg and the sac swells up with fluid.
- A luteal cyst. This type occurs when the sac releases an egg and then reseals and fills with fluid.
What causes them?
A functional ovarian cyst is caused by slight changes in the way the ovary makes or releases an egg. A cyst may form when a sac on the ovary doesn't release an egg, and the sac swells with fluid. Or the sac may release an egg and then reseal and fill with fluid.
What are the symptoms?
Most functional ovarian cysts don't cause symptoms. The larger the cyst is, the more likely you'll have symptoms. Symptoms include pelvic pain, pain with intercourse, lower belly pain, and changes to your period.
How are they diagnosed?
If you see your doctor for pelvic pain or bleeding, you'll be checked for problems that may be causing your symptoms. Your doctor may find an ovarian cyst during a pelvic exam. You may have a pelvic ultrasound to see if the cyst is filled with fluid.
How are functional ovarian cysts treated?
Most functional ovarian cysts go away without treatment. Your doctor may suggest using heat and medicine to relieve minor pain. Surgery can remove a large cyst that bleeds or causes severe pain. Your doctor may suggest that you take birth control pills, which stop ovulation. This may prevent new cysts from forming.
What Increases Your Risk
A functional ovarian cyst sometimes develops near the end of the menstrual cycle, when an egg follicle fills up with fluid. Factors that may increase your risk for developing a functional ovarian cyst include:
- A history of a previous functional ovarian cyst.
- Current use of medicine to start ovulation.
- Use of low-dose progestin-only contraception (such as some implants, pills, and IUDs).
Learn more
Symptoms
Functional ovarian cysts usually are harmless and don't cause symptoms. The larger the cyst is, the more likely it is to cause symptoms. Symptoms may include:
- Pelvic pain.
- Pain with intercourse.
- Belly pain.
- Menstrual period changes.
There are many other conditions that cause symptoms like those of a functional ovarian cyst. So it's important to have any unusual pelvic symptoms checked and to have a pelvic exam.
What Happens
Most functional ovarian cysts cause no symptoms and go away after 1 to 2 menstrual periods. Some cysts grow as large as 10 cm (4 in.) in diameter before they shrink or rupture. They don't cause ovarian cancer.
When to Call a Doctor
Call your doctor now if you have:
- Sudden, severe pelvic pain with nausea or vomiting.
- Severe vaginal bleeding.
- Sudden faintness or weakness.
- Sudden dizziness with belly discomfort that lasts for 2 hours or longer.
Call your doctor for an appointment if:
- Pain interferes with your daily activities.
- Your periods have changed from relatively pain-free to painful during the past 3 to 6 months.
- Your periods have changed from regular to infrequent during the past 3 to 6 months and you aren't nearing menopause.
- You have pain during sexual intercourse.
Watchful waiting
Most functional ovarian cysts are harmless, don't cause symptoms, and go away without treatment. Watchful waiting is usually okay if you are diagnosed with a functional ovarian cyst.
Check your symptoms
Exams and Tests
If you see your doctor for pelvic pain or bleeding, you'll be checked for problems that may be causing your symptoms. Your doctor will ask you about your symptoms and menstrual periods.
Your doctor may find an ovarian cyst during a pelvic exam. You may have a pelvic ultrasound to see if the cyst is filled with fluid.
Your doctor may recommend further testing in some cases, such as when the first ultrasound doesn't clearly show what kind of cyst or growth you have. Or other tests may be done if you have moderate to severe pain or vaginal bleeding.
What do ovarian cysts look like on ultrasound?
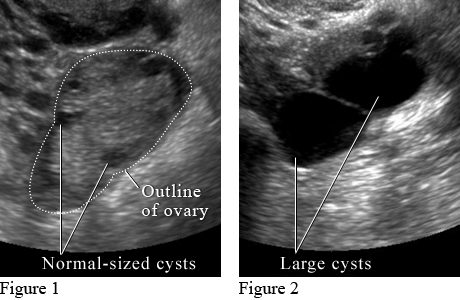
Image courtesy of Intermountain Medical Imaging, Boise, Idaho.
Figure 1 shows small normal-sized cysts. Figure 2 shows large cysts that affect the ovary and may cause pain.
Learn more
Treatment Overview
Most functional ovarian cysts go away without treatment. When treatment is needed, the goals are to:
- Relieve pelvic pain or pressure.
- Prevent more cysts from forming.
Home treatment with heat and pain medicine can often relieve symptoms.
Treatment with medicines or surgery may be used for a cyst that doesn't go away, looks odd on an ultrasound, or causes symptoms.
Your doctor may suggest that you try birth control pills for several months. They prevent ovulation. This can stop more cysts from forming.
Surgery to remove the cyst (cystectomy) through a small incision (laparoscopy) may be done. This is done if a painful cyst doesn't go away with treatment. If a cyst looks odd on an ultrasound or if you have other risk factors for ovarian cancer, your doctor may recommend surgery to remove the cyst through a larger belly incision (laparotomy).
Learn more
Watch
Self-Care
- Use heat, such as a hot water bottle, a heating pad set on low, or a warm bath, to relax tense muscles and relieve cramping.
- Be safe with medicines. Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- Avoid constipation. Make sure you drink enough fluids and include fruits, vegetables, and fibre in your diet each day. Constipation does not cause ovarian cysts, but it may make you feel more uncomfortable.
Learn more
Credits
Current as of: April 30, 2024
